Neurology
EM Quick Hits 6 Blunt Cardiac Trauma, Atrial Fibrillation Anticoagulation, Hydromorphone vs Morphine, Myasthenia Gravis, Venous Access
In this EM Quick Hits episode: Andrew Petrosoniak on diagnosis and risk stratification of blunt cardiac trauma, Clare Atzema on latest guidelines for anticoagulation in atrial fibrillation, Maria Ivankovic on hydromorphone vs morphine for acute pain, Brit Long on clinical pearls in the diagnosis of myasthenia gravis, Anand Swaminathan on venous access tips and tricks, and bonus material from EM Cases Course June 2018 with Walter Himmel and Barbara Tatham on Physician Compassion and tools to prevent burnout...
Ep 120 ED Stroke Management in the Age of Endovascular Therapy
In this EM Cases main episode podcast, a follow up to our episode on TIA released in November 2018 with Walter Himmel and David Dushenski, we’ll try to simplify the confusing time-based and brain tissue-based options for stroke management. We’ll answer the questions that have been plaguing us for a while now: Which patients are eligible for endovascular therapies? Which patients are the ones who’ll benefit from these therapies and how do we make that happen in our different practice environments? Which patients should be considered for lytic therapy? Which patients should be considered for both lytic and endovascular therapy? and many more...
Ep 117 TIA Update – Risk Stratification, Workup and Dual Antiplatelet Therapy
Much has changed in recent years when it comes to TIA risk stratification, workup and antiplatelet therapy. In this podcast we use the overarching theme of timing to elucidate how to distinguish true TIA from the common TIA mimics, the importance of timing in the workup of TIA, why the duration of therapy with dual antiplatelet therapy and timing of starting anticoagulation in patient with atrial fibrillation, contributes to the difference between preventing catastrophic strokes and causing intracranial hemorrhage...
CritCases 10 Hyponatremia Associated Seizures
In this EM Cases CritCases blog - a collaboration between STARS Air Ambulance Service, Mike Betzner and EM Cases, a middle aged woman presents to a rural ED with headache and vomiting, normal vital signs with subsequent status epilepticus and serum sodium of 110 mmol/L. What management recommendations would you make to the rural ED physician, the transport team and in your ED with regards to treatment of seizures, safe correction of hyponatremia, airway management, search for underlying cause and prevention of Osmotic Demyelenation Syndrome?
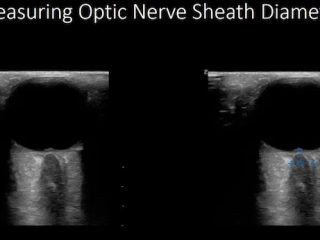
POCUS Cases 3 Idiopathic Intracranial Hypertension and Ocular POCUS
In this POCUS Cases 3 - Idiopathic Intracranial Hypertension & Ocular POCUS, Dr. Simard explains the limitations of CT head in the diagnosis of idiopathic intracranial hypertension, how to identify papilledema on ocular POCUS, how to measure Optic Nerve Sheath Diameter (ONSD) on POCUS and the limitations of ONSD on ocular POCUS.
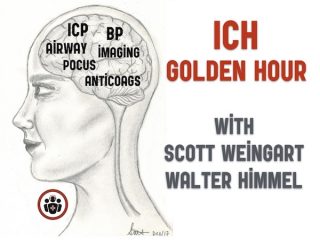
Ep 104 Emergency Management of Intracerebral Hemorrhage – The Golden Hour
There exists a kind of self-fulfilling prognostic pessimism when it comes to ICH. And this pessimism sometimes leads to less than optimal care in patients who otherwise might have had a reasonably good outcome if they were managed aggressively. Despite the poor prognosis of these patients overall, there is some evidence to suggest that early aggressive medical management may improve outcomes. As such, the skill with which you manage your patient with ICH in those first few hours could be the most important determinant of their outcome. In this Golden Hour you have a chance to prevent hematoma expansion, stabilize intracerebral perfusion and give your patient the best chance of survival with neurologic recovery.