emergency medicine toxicology
Episode 90 – Low and Slow Poisoning
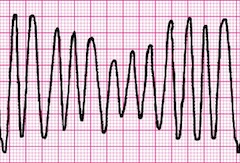
One of the things we need to think about whenever we see a patient who’s going low and slow with hypotension and bradycardia is an overdose. B-blockers, calcium channel blockers (CCB) and digoxin are some of the most frequently prescribed cardiovascular drugs. And inevitably we’re gonna be faced with both intentional and unintentional overdoses from these drugs in the ED. If we can recognize these overdoses early and manage them appropriately, well - we’ll save some lives...