emergency medicine neurology
CritCases 8 Management of Elevated ICP
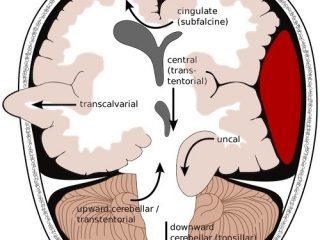
In this CritCases blog - a collaboration between STARS Air Ambulance Service, Mike Betzner and EM Cases, we take you through a not uncommon stroke presentation which then develops into a challenge with regard to management of elevated ICP, hypertension and the airway...