emergency medicine education
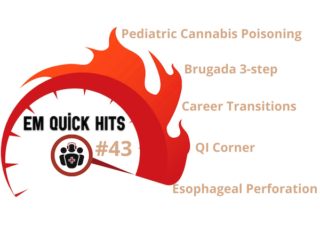
EM Quick Hits 43 Pediatric Cannabis Poisoning, Esophageal Perforation, Brugada, Career Transitions in EM
On this month's EM Quick Hits podcast: Best of University of Toronto EM with Yaron Finkelstein on pediatric cannabis poisoning pitfalls, Brit Long on recognition and management of esophageal perforation, Jesse McLaren on 3 questions to diagnose Brugada Syndrome, Tahara Bhate on QI Corner, Constance Leblanc on maintaining wellness in career transitions from CAEP 2022...